ReVIDA® Recovery: How Opioids Are Impacting Tennessee Residents’ Lives
Opioids have been present in the medical field in the United States since 1898, with the introduction of heroin as a “less habit-forming morphine.” Over the years, we’ve learned more about them, from outlawing heroin in the 1910s to the controlled substances act being passed in the 1970s. The CDC, however, pinpoints the start of the current opioid epidemic to about the 1990s due to the introduction of new, prescription opioids like OxyCotnin. In recent years, we’ve realized some of the risks and downfalls associated with long-term or high-quantity opioid use.
In 2018 alone, the University of Tennessee Medical Center filled over 1.46 million opioid prescriptions. In Knox County, there were over 347,000 prescriptions filled. This doesn’t account for misuse or opioids procured through illegal means, either. While not all prescriptions should be considered inherently bad, knowing how many prescriptions were filled can be important when looking at the opioid situation here in Tennessee. Opioids come with the risk of addiction, even when taking it as directed.
Our goal here at ReVIDA® Recovery is to help our community feel empowered to reclaim their lives from opioid use. We’ve seen recovery happen time and time again. The purpose of this guide is to further look at the opioid crisis occurring in our country and state and to talk about the steps we can take to help better our communities.
It’s Not Just Tennessee – A Look at Nationwide Opioid Use
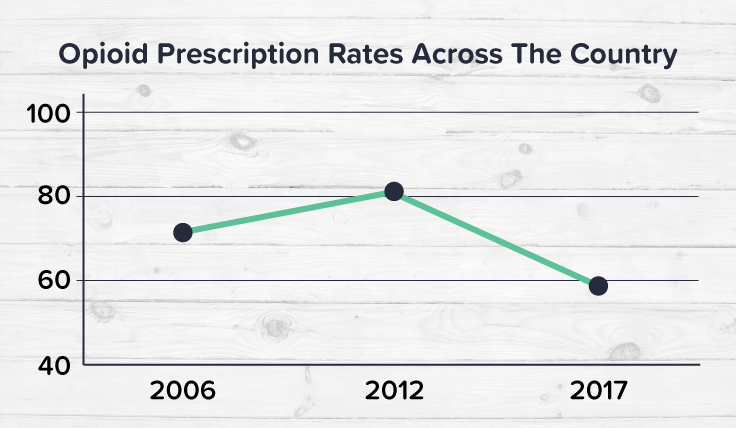
When looking at opioid prescriptions across the country from 2006-2018, we can see that prescription rates overall have started to slowly decline. Starting at 72 prescriptions per 100 people in 2006, peaking at over 81 prescriptions per 100 in 2012, and declining since then with 2017 sitting at just under 59 prescriptions. This is a good trend to see, as we have seen that prescription opioids can contribute to opioid use disorders, but there’s more to it.
Heroin and Fentanyl’s Contribution to the Crisis
Heroin and fentanyl are both opioids. Heroin is an illegal opioid crafted from morphine, and fentanyl is a synthetic, highly potent opioid used to treat severe pain.
While opioid-related deaths took a small hit in 2012, when we started to see the beginnings of limiting opioid use, heroin has had no such dip. It has steadily increased in prevalence over the past decade.
Fentanyl use and overdoses have skyrocketed in the past 5 years. Due to the ease with which drug dealers can access fentanyl, and because of its high potency, many drug dealers have been lacing other substances with fentanyl. This cuts back on costs for them while still giving the person buying the substance a high. The problem comes, however, from the person being unaware of fentanyl’s presence. Because it is so much more potent, they often take their usual dosage without realizing that the fentanyl is present, leading to an increased risk of overdose.
Since 1999, the amount of deaths related to opioid use has quickly increased. What impacted these numbers the most, has been heroin and fentanyl. From 2010 to 2017, deaths related to heroin use increased by 500%. Fentanyl has had the largest jump. Starting in 2013, deaths related to synthetic opioids jumped from 1 per every 100,000 people to 10 by 2017. This is a 1000% increase.
How Appalachia Is Impacted by Opioids
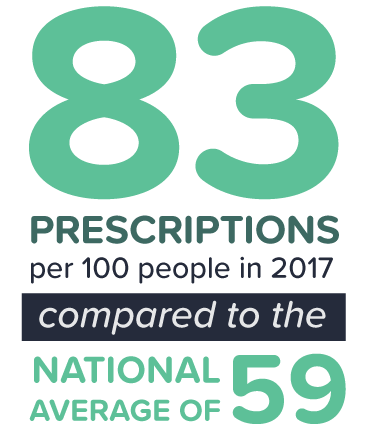
Did you know that Tennessee and the Southeast as a whole have some of the highest rates of opioid prescriptions in the country? Tennessee sits at approximately 83 prescriptions per 100 people in 2017 compared to the national average of 59.
There’s a reason for this, and it doesn’t just occur here in Tennessee, but in many parts of Appalachia. Studies have shown that there is a correlation between opioid use and people who received serious injuries at work. Coal mining is one of the jobs in the United States with the highest percentage of injuries, with manufacturing jobs being another.
Overdose mortality rates are higher in Appalachia than in other parts of the United States, with Appalachia sitting at just over 20 deaths per 100,000 to the nationwide average of just over 14 deaths per 100,000. Why exactly is that? What factors in daily life in Appalachia contribute to this increase?
Coal Mines, Labor, and Opioids
Coal mining has a long history in Appalachia. In fact, it was the primary source of coal production in the United States from the 1800s all the way through the 1970s. Coal mining has decreased in prevalence in Appalachia only in numbers. Its history is still strongly rooted there. In 2010, over 56,000 people were working in coal mines. As of 2021, however, that number has decreased to about 22,000.
Despite the decrease in workforce presence, this career path still isn’t known for its safety. It has a high rate of injury, as we talked about above. What exactly is the correlation between workplace injuries and opioid use, though?
In a study of over 46,000 workers in Tennessee who both experienced a workplace injury and were previously opioid-free – 1,800 of them (or 4%) began long-term opioid use. With coal mining being one of the highest-risk jobs in the United States, combined with the correlation between workplace injuries and developing an opioid dependency, the chance of someone developing an opioid use disorder in Appalachia is higher than in some other places in the United States.
Where Tennessee Stands in the Opioid Crisis
There are many contributing factors that add to Tennessee’s opioid epidemic. How exactly is the state being impacted? Are there certain regions that are seeing higher rates of overdose and misuse than others? Are there things we could work on to help lower these numbers? What are the trends and is there a way we can address them?
Opioid Use by Demographic
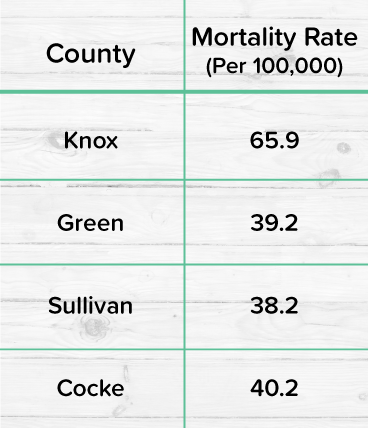
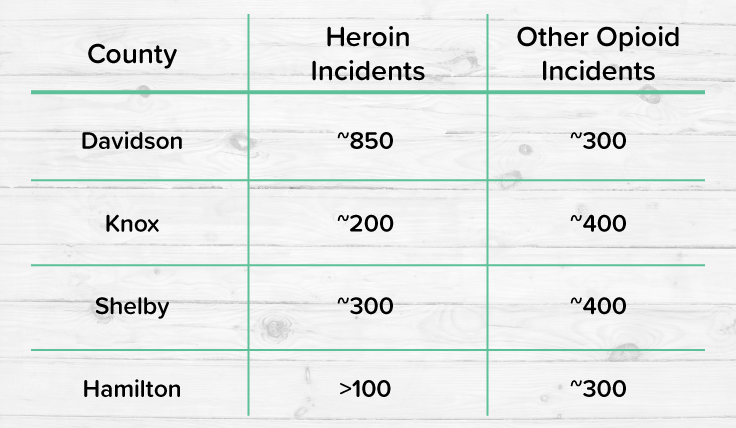
On average, the overdose mortality rate in Tennessee is about 38 people per 100,000. This means about 2.6k people die in Tennessee each year from opioid overdoses. If you look at the state on a county-to-county basis, however, you will find that some counties have higher rates of overdose mortality per 100,000 people than others.
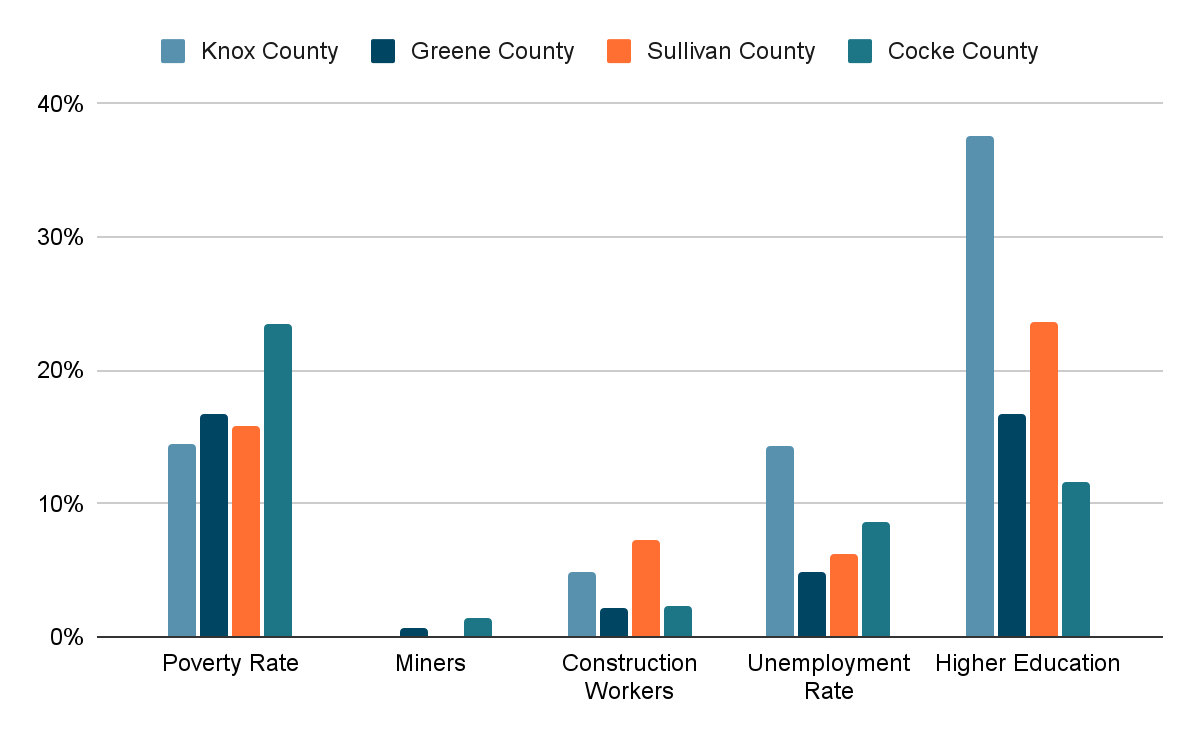
What changes between these counties impact these numbers? Let’s take a look at some of the population statistics for these counties.
Source: https://overdosemappingtool.norc.org/
While there are some conclusions that could be drawn from this data, such as unemployment rates correlating with opioid use, not every category shows a clear pattern.
Now you might want to try to draw a conclusion that Knox county has the highest rate of people with higher education, but Sullivan county is second highest on our list while holding the lowest mortality rate of all four counties.
Opioid Overdoses in Tennessee
Let’s take a closer look at the breakdown of opioid overdose by age group:
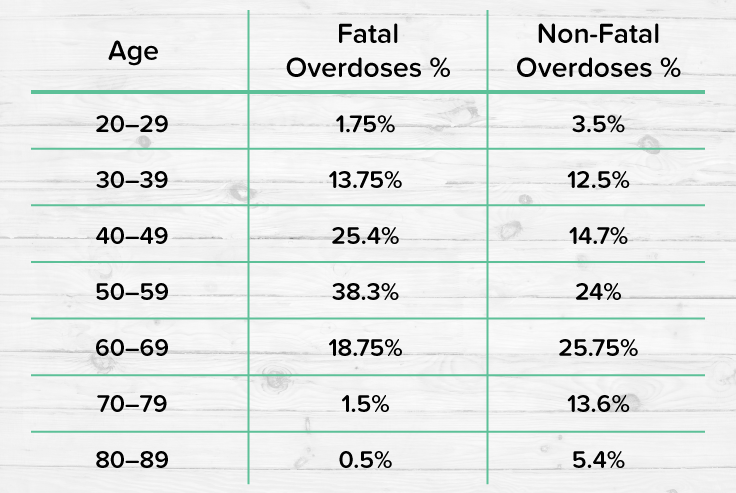
As you can see, there’s not just one age group that’s impacted by opioid use. In fact, while most substance use generally has a higher percentage of young adults that are afflicted by it, you can see that opioid use impacts a larger audience. Due to pain medication sometimes being needed more often as you get older, there are many adults and geriatric people who also might be managing opioid use.
Prevention and Prediction – What Can We Do About Opioid Use?
After looking at the data above, it’s not uncommon to want to draw a conclusion. The problem is – substance use isn’t a formula. While there are many factors that can contribute to substance use, from age and poverty to education level and family history, none of these factors guarantee specific results. An OUD requires a medical diagnosis, so even if you are ticking off multiple boxes for an increased risk, you may still not have one.
This doesn’t mean that there’s no way to prevent future opioid use, nor that there isn’t a way to continue to lower the overdose cases that occur here in Tennessee each year. Here at ReVIDA® Recovery, we’re always taking steps to fill the unmet opioid use disorder treatment needs of our communities. Recovery is possible, and we see it happen all the time, but prevention is just as important. These are just some of the steps we’re taking to help our communities:
- Destigmatize substance use – Helping lower the stigma around substance use can not only help people find help quicker but also make conversations about substance use easier to have.
- Provide educational, easy-to-access information on substance use – When people are more informed about what’s going into their bodies, what’s occurring in their bodies, and what they can do to help themselves, they’re able to make informed decisions about their health and well-being.
- Make life-saving medication more easily accessible – There are medications that can help assist in the case of an opioid overdose, medications that are life-saving. Making sure our communities have access to these medications can help save lives.
- Partner with the community to offer resources to all – Our patients mean the world to us, and our communities are an extension of that. Through many fantastic partnerships, we can help our patients find what they need during and after recovery, from careers to housing and family support.
Spotting the Signs of an Opioid Use Disorder
Opioids work by binding to the opioid receptors in our cells. These receptors are found throughout the brain, spinal cord, and other parts of the body and allow us to experience feelings of both pain and pleasure. When an opioid is present in the body, it blocks these receptors from feeling pain. It then also triggers the release of excess dopamine. This combination has the potential to encourage continued consumption outside of your prescription. Taking opioids in a way other than how they’re prescribed is one of the many signs of a potential opioid dependency or opioid use disorder.
When patients are unable to cut back on opioid use, they’re seeking it through means beyond their doctor, or if their opioid use is starting to impact a large portion of their life – they might have an opioid use disorder.
How ReVIDA® Can Help You Find Recovery From Opioid Use
There are many people here in Appalachia who are looking to change the path their life is currently on and ReVIDA® Recovery is here to help. Sometimes the most difficult part can be that first step. It can seem daunting, but we’ve seen patients time and time again reclaim their lives from opioids.
Helping a Loved One Who Has an Opioid Use Disorder
When the family members of our patients realize their loved one might be managing a substance use disorder, this can scare them. We do our best to help not only our patients during recovery but their family members as well. It’s not uncommon for us to receive calls from loved ones, concerned about their spouse or friend in regard to opioid use. That’s why we’ve made this list to help them out as well.
Let’s go through some Do’s and Don’ts:
DO
- Remind them that you care
- Be a good listener
- Offer to help in whatever way they want
- Celebrate small victories with them
- Be supportive and encouraging
DON’T
- Judge them for their choices
- Make them feel like it’s their fault
- Berate or belittle them if they make a mistake
Our Mission
One of our most important goals here at ReVIDA® Recovery is to ensure that our patients know that they’re not just a number to us. Everyone who walks through our door is an individual. Our patients are more than just their substance use. Each patient’s journey is unique, and we understand that.
We strive to offer a safe and healthy place for people to find the healing they’re looking for. We believe in working alongside our communities to make sure our patients have their needs met. We want to see our patients continue to succeed outside of our facilities.
Our Treatment Programs
We offer three primary services here at ReVIDA® to help along the path of recovery and healing. All of our programs are evidence-based and industry-leading to ensure that our patients have access to the best care possible.
- Medication-Assisted Treatment (MAT) – Our MAT programs are designed to help alleviate withdrawal symptoms so patients can start focusing on their recovery. They’re a tool to start the journey. During MAT our patients are closely monitored by our knowledgeable and compassionate staff. We use a combination of medication and traditional therapy to help guide them away from opioid use and onto the path of recovery.
After MAT, their clinician will help assess the best options for that specific patient’s continued treatment. Not everyone has the same needs, so we’ll help find what’s best on an individual level. At ReVIDA® we also have outpatient programs for continued care and recovery. If a higher level of care is needed, we can also provide referrals to local inpatient or residential programs.
- Buprenorphine (Suboxone®) Treatment – Buprenorphine (Suboxone®) is another branch of treatment that we offer here at ReVIDA® Recovery. It has been proven to reduce opioid cravings and works to help prevent potential relapse. It’s a great tool to have during recovery. In order to be eligible for buprenorphine (Suboxone®) treatment a patient must be opioid-free for 24 hours.
- Outpatient Rehab Services – Our outpatient services offer both individual and group therapy, which are critical components for treating an OUD. Having these two work together can help establish a strong base for recovery. While here, our patients go through the 12-step program, learning how to manage triggers and find healthy coping mechanisms. Our team is full of medical professionals who are passionate about what they do – from licensed therapists to care coordinators, we have staff who can help every step of the way.